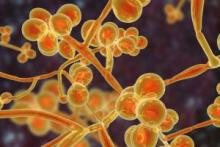
Candida auris
General Information:
Candida auris (CAUR) is a multi-drug-resistant fungal pathogen that can cause healthcare-associated infections and outbreaks and, therefore, poses a serious threat to global human health. CAUR can also colonize patients without causing infection. Invasive CAUR infections can lead to severe morbidity and mortality, especially among hospitalized patients who are immunocompromised and or receiving intensive care. Mortality rates of invasive CAUR infections are estimated to be greater than 40%.
CAUR has spread in hospitals and long-term care (LTC) settings across the globe. Multiple healthcare-associated CAUR outbreaks and the identification of pan-resistant CAUR isolates internationally have increased concerns about the impacts of CAUR in healthcare settings.
The World Health Organization (WHO) considers CAUR to be a critical fungal pathogen on the WHO fungal priority pathogens list and a public health threat that requires urgent and aggressive action.
Transmission
CAUR is highly transmissible between patients through contact with contaminated surfaces or objects and hands of healthcare workers. Infected and colonized patients can shed CAUR on objects and surfaces around them including bedrails, doorknobs, and mobile medical equipment. CAUR can live on surfaces for long periods of time making it harder to keep surfaces disinfected. Patients have been found to be colonized for a long time after active infection has resolved. The maximum duration of colonization with CAUR is not known. There are currently no efficacious strategies for decolonization.
Symptoms
CAUR infections are nonspecific and depend on the location and severity of infection. The most common symptoms include fever and chills as with most bacterial infections. Clinical infections may require antifungal therapy. Patients with invasive medical devices are more likely to get infected with CAUR such as critically ill patients in ICUs. The spectrum of CAUR infection ranges widely from superficial skin infection to invasive disease. Non-invasive infections associated with CAUR include respiratory tract infections, urinary tract infections, otitis externa, wound infections, and skin abscesses (often related to catheters). Invasive infections associated with CAUR include bloodstream infections, pericarditis, myocarditis, meningitis, and osteomyelitis.
Diagnosis
CAUR can be difficult to distinguish from other Candida species in the laboratory. Culture-based methods may take days to obtain the results and may lack sensitivity. The most reliable way to identify CAUR is by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) and polymerase chain reaction (PCR).
Infection Prevention in Healthcare Settings:
Infection control measures for CAUR in acute care hospitals and high acuity post-acute care settings include:
- Use of a single-patient room and standard and contact precautions
- Hand hygiene adherence
- Cleaning and disinfection of the patient care environment and reusable equipment (daily and terminal cleaning) using an Environmental Protection Agency (EPA)–registered hospital-grade disinfectant effective against CAUR. In the US, see EPA’s List P or List K or in Canada use a Health Canada-approved healthcare disinfectant with claims of efficacy against C. auris.
- Screening of contacts of newly identified cases to identify CAUR transmission
- Full investigation of every new case
- Implementation of a surveillance program based on local epidemiology
- Ensure inter-facility communication of patient’s CAUR status when transferring patients between healthcare facilities
Environmental Cleaning and Disinfection:
Thorough daily and terminal cleaning and disinfection of patients’ rooms and cleaning and disinfection of areas outside of their rooms where they receive care (e.g., radiology, physical therapy) is necessary. Perform cleaning and disinfection of frequently touched environmental surfaces and shared equipment using EPA-registered or Health Canada-approved products with label claims for use in healthcare. Follow the manufacturer’s recommendations for application and contact times. Accumulating data indicates that products solely dependent on quaternary ammonia compounds (QACs) are NOT effective against CAUR.
CAUR can persist on surfaces in healthcare environments for prolonged periods of time and has been cultured from multiple locations in patient rooms, including both high-touch surfaces, such as bedside tables and bedrails, and locations further away from the patient, such as windowsills. CAUR has also been identified on mobile equipment, such as glucometers, temperature probes, blood pressure cuffs, ultrasound machines, nursing carts, and crash carts. Meticulous cleaning and disinfection of both patient rooms and mobile equipment is necessary to reduce the risk of transmission. Increased cleaning and disinfection (i.e. twice daily) is recommended especially during an outbreak.
The following are Diversey disinfectants with claims against CAUR:

References:
Candida auris Infection Prevention and Control in Canadian Healthcare Settings, December 2024: https://www.canada.ca/en/services/health/publications/diseases-conditions/candida-auris-infection-prevention-control-canadian-healthcare-settings.html
CDC Infection Control Guidance: Candida auris: https://www.cdc.gov/candida-auris/hcp/infection-control/index.html
Public Health Ontario Focus on Candida auris June 2023: https://www.publichealthontario.ca/-/media/Documents/C/2023/candida-auris.pdf?rev=c598e884d26140ee8c78d91057c234f2&sc_lang=en

