
Clostridioides difficile
General Information
Clostridioides difficile [klos–TRID–e–OY-dees dif–uh–SEEL] is formerly known as Clostridium difficile and often called C. difficile or C. diff. C. diff is a germ (bacterium) that causes diarrhea and colitis (an inflammation of the colon).
People who have other illnesses or conditions requiring prolonged use of antibiotics and the elderly, are at greater risk of acquiring this disease. The bacteria are shed in the feces.
People can become infected if they touch items or surfaces that are contaminated with feces and then touch their mouth or mucous membranes. C. difficile infections (CDI) can cause: pseudomembranous colitis (PMC), toxic megacolon, perforations of the colon, sepsis, and death.
Significance
According to the CDC, C. diff is a major health threat. C. diff infection is estimated to cause almost half a million illnesses in the United States each year, and an estimated 29,300 deaths (Guh et al, 2020). In Canada, there are approximately 3.8 cases per 10,000 patient days in 2020 (CNISP), and a mortality rate of 1.3-2.7% in cases.
Symptoms
Symptoms include watery diarrhea (at least three bowel movements per day for two or more days), fever, loss of appetite, nausea, and abdominal pain/tenderness.
Transmission
C. difficile is shed in feces. Most patients remain asymptomatic after infection. The organism can form spores when growth conditions are unfavorable, and these spores enables the pathogen to persist in the environment for extended periods of time (e.g., in soil and on dry surfaces). Any surface, device, or material (e.g., toilets, bathing tubs, and electronic rectal thermometers – a disposable thermometer should be used for hospitalized patients) that becomes contaminated with feces may serve as a reservoir for the C. diff. spores. Environmental surfaces may serve as a reservoir for transmission of the spores. Spores are transferred to patients mainly via the hands of healthcare personnel who have touched a contaminated surface or item.
Risk Factors
Risk factors of acquiring infection include: antibiotic exposure (especially fluoroquinolones, third/fourth generation cephalosporins, clindamycin, carbapenems), gastrointestinal surgery/manipulation, long length of stay in healthcare settings, serious underlying illness, immunocompromising conditions and advanced age
Treatment
In about 20% of patients, CDI will resolve within 2-3 days of discontinuing the antibiotic to which the patient was previously exposed. The infection can usually be treated with an appropriate course (about 10 days) of antibiotics.. After treatment, repeat C. difficile testing is not recommended if the patients’ symptoms have resolved, as patients may remain colonized. Prescribing providers are encouraged to review the Infectious Disease Society of America’s most recent treatment guidelines (https://www.idsociety.org/practice-guideline/practice-guidelines/#/+/0/date_na_dt/desc/).
Treatment is generally not recommended for patients with asymptomatic C. diff colonization, as this may put them at risk for development of other multidrug resistant organisms (MDROs).
General Prevention Guidelines
Per the CDC, healthcare professionals can help prevent C. diff by:
- Optimizing antimicrobial prescribing & engaging in the facility’s Antimicrobial Stewardship Program
- Using diagnostic testing methods that provide the most accurate results, including testing only those patients who meet facility testing criteria
- Rapidly isolate and initiate contact precautions for suspected or confirmed diff
- Wearing gloves and gowns when caring for patients suspect or confirmed with diff
- Cleaning surfaces in rooms where diff patients are treated with EPA-approved, spore-killing disinfectant (see EPA’s List K, available at https://www.epa.gov/pesticide-registration/list-k-antimicrobial-products-registered-epa-claims-against-clostridium).
Maintain contact precautions per facility transmission-based isolation policies and procedures.. If the patient/resident remains in the healthcare setting after the diarrhea resolves, consider transfer to a new room and perform terminal disinfection of the previously occupied room. Monitor patients/residents potentially exposed to C. diff prior to initiation of contact precautions.
Some healthcare facilities may place suspect/confirmed C. diff patients into “enteric” or “plus” contact precautions, using signage that is different from general contact precautions. Distinguishing C. diff isolation from generic contact isolation may support targeted use of sporicidal disinfectants and remind staff to use soap and water for hand hygiene after potential exposure to feces. Healthcare providers should refer to their individual hand hygiene policy for further guidance.
Cleaning and Disinfection
Proper cleaning and disinfection is critical in reducing the risk of C. diff transmission.
It is recommended to use a sporicidal agent to address environmental contamination in the rooms of patients known or suspected to have active C. difficile (CDC 2019). Also, sporicidal agents can be used in areas associated with increased rates (hyperendemic) of CDI or in outbreak situations.
For cleaning and disinfection against C. diff, it is encouraged to carefully read the label. Some products require a 2-step cleaning and disinfection process (clean first and then disinfect) and others require the removal of gross/visible soil prior to disinfection.
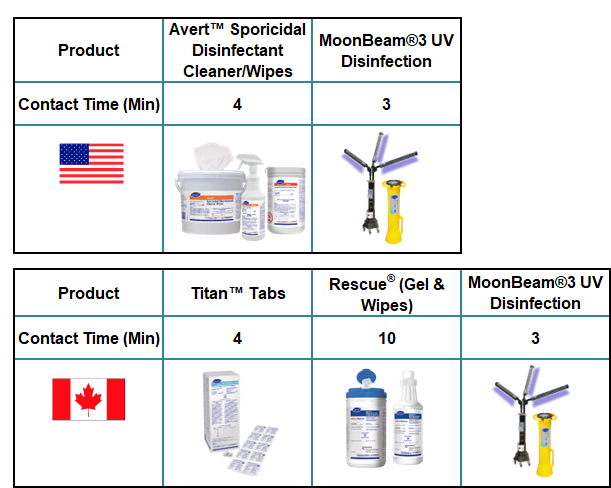
Clostridioides difficile is susceptible to the following Diversey disinfectants and devices:
References:
Guh AY, Mu Y, Winston LG et al. N Engl J Med 2020;382:1320–30. DOI: 10.1056/NEJMoa1910215.
The Canadian Nosocomial Infection Surveillance Program CNISP) https://health-infobase.canada.ca/cnisp/hai-aro-rates.html Current to Nov 18, 2022. Accessed June 16, 2023.
Canadian Nosocomial Infection Surveillance Program. Healthcare-associated infections and antimicrobial resistance in Canadian acute care hospitals, 2016–2020. Can Commun Dis Rep 2022;48(7/8):308–24. https://doi.org/10.14745/ccdr.v48i78a03
CDC. Clostridioides difficile Fact Sheet. Available at https://www.cdc.gov/cdiff/pdf/Cdiff-Factsheet-P.pdf.
CDC. 2021. Strategies to Prevent Clostridioides difficile Infection in Acute Care Facilities. Available at https://www.cdc.gov/cdiff/clinicians/cdi-prevention-strategies.html

