General Information
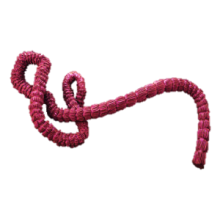
Ebola virus disease (EVD) or Ebola hemorrhagic fever (Ebola HF) is a disease caused by the Ebola Virus, an enveloped virus. Ebola Virus Disease (EVD) is a rare and deadly disease in people and nonhuman primates. The viruses that cause EVD are located mainly in sub-Saharan Africa. People can get EVD through direct contact with an infected animal (bat or nonhuman primate) or a sick or deceased person infected with Ebola virus.
Symptoms
When infection occurs, symptoms usually begin abruptly. Symptoms of EVD include fever, severe headache, joint and muscle aches, weakness, diarrhea, vomiting, stomach pain, lack of appetite, and abnormal bleeding. Symptoms may appear anywhere from 2-21 days after exposure to the Ebola virus, although 8-10 days is most common.
In approximately half of the patients, the disease becomes severe, causing bleeding. These patients may vomit blood, pass blood through their urine, or bleed under the skin or from their eyes and/or mouth. Death occurs when vessels deep in the body begin leaking fluid, causing a drastic drop in blood pressure which ultimately leads to multi-organ (heart, kidneys, liver, and other organs) failure. The fatality rate is estimated at 40-90%.
Transmission
The infection is transmitted by direct contact with blood, body fluids or tissue of infected animals or people. Patients can transmit the virus after showing symptoms and also postmortem. According to infectious disease experts at the WHO and the CDC, the virus is transmitted through direct contact with the blood and body fluids of an infected symptomatic person or through direct contact with objects that have been contaminated with infected secretions (i.e. needles).
The infection can enter the body through open wounds or mucous membranes such as the mouth, nose, or eyes. The virus is also able to survive on contaminated surfaces, so objects contaminated with blood or body fluids such as gloves and needles may be a source of disease transmission. Ebola is not transmitted through the air, food, or water.
In outbreak settings, Ebola virus is typically first spread to humans after contact with infected wildlife and then is spread person-to-person through direct contact with blood and other body fluids, including sweat, semen, and breast milk. The disease can also be spread postmortem when a person could become infected by touching the body during funeral preparations.
During an outbreak, those at higher risk of infection are health workers, family members, and others in close contact with infected and deceased patients. Unfortunately, healthcare personnel are at high risk of acquiring the infection, especially if the use of PPE (Personal Protective Equipment) is not used correctly.
Treatment
There are currently two treatments approved by the U.S. Food and Drug Administration (FDA) to treat EVD caused by the Ebola virus, species Zaire ebolavirus, in adults and children.
Prevention
The likelihood of contracting Ebola in North America is considered extremely low unless there is direct exposure to the body fluids of an infected person or handling and eating the meat of infected animals/bats. Ebola is not spread through casual contact; therefore, the risk of an outbreak in North America is very low. The CDC has reinforced that EVD can be controlled through the use of recommended protective measures in clinics and hospitals. Early recognition
and identification of patients with potential EVD is critical.
Hospitals have been directed to follow Standard, Contact/Airborne precautions for the management of hospitalized patients with known or suspected Ebola virus disease (EVD). It is advised that if you will be traveling to Africa go to CDC.gov to find out if there are current travel restrictions in place.
Guidelines and Recommendations
Any hospital with suspected patients should follow CDC’s Recommendations for Hospitalized Patients with Known or Suspected Ebola Hemorrhagic Fever in Hospitals. https://www.cdc.gov/vhf/ebola/clinicians/cleaning/hospitals.html
Detailed guidelines and recommendations are available at the following links:
WHO:
CDC:
- http://www.cdc.gov/vhf/ebola/hcp/infection-prevention-and-control-recommendations.html
- http://www.cdc.gov/vhf/ebola/hcp/environmental-infection-control-in-hospitals.html
- https://www.cdc.gov/vhf/ebola/history/chronology.html
FDA
Cleaning and Disinfection of Environmental Surfaces
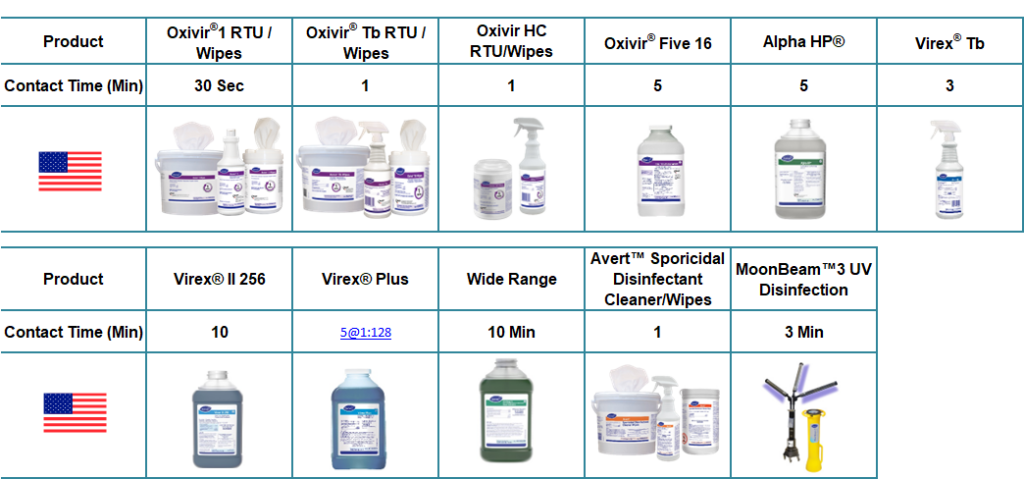
The following disinfectants qualify based on the above EPA and PHAC (Public Health Agency of Canada) recommendations as disinfectants.
An EPA-registered hospital disinfectant with label claims against Ebola on List L, or Emerging Viral Pathogens for Tier 1, non-enveloped viruses should be used for disinfection. These are published on List Q.
The EPA List Q Emerging Viral Pathogens includes the following (Ebola is considered a Tier 1):
References: See guidelines and recommendations noted in the body of this document.

