Ready to throw in the towel?
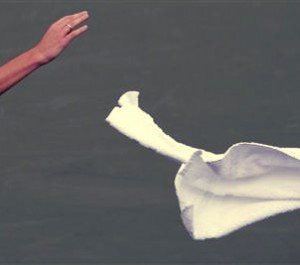
Maybe you should be…
A new study shows that ready-to-use disinfectant wipes increase compliance while saving time and money.
Selecting the right disinfectant and cleaning tools can be a real challenge in a healthcare setting. There are numerous criteria that need to be taken into consideration when you are designing your cleaning and disinfecting program, and as you’ll see below a simple cleaning tool can be a complex variable in the effectiveness of your program. Here are some considerations…
Compatibility Between Cleaning Tools and Disinfectants – Some cleaning tools, such as cotton cloths and microfiber, can bind with quaternary ammonium compounds (quats), reducing the efficacy of the disinfection process. One of the key benefits of ready-to-use disinfectant wipes is that there is no need to determine if the tool will work with the disinfectant – the efficacy testing has been done on the disinfectant/tool combination, so no additional guess work is required.
Laundering – Reusable cloths require collection, laundering and/or reprocessing. Some facilities have the capability to do this within their system, while others need to outsource this task. Either way, it is a major responsibility to ensure that the quality of the laundering process meets your requirements. Studies have shown that ineffective laundering processes can lead to cleaning cloths and mops that aren’t really clean, and in some cases, they have been linked to the transmission of infection and outbreaks. Ready-to-use wipes eliminate the need for laundering and its associated risks, labor and cost.
Cross Contamination –Cross contamination can happen when dirty cleaning cloths are dipped into clean disinfectant solution, contaminating the entire solution. Another issue is that a cleaning cloth can become contaminated throughout its use or within the facility, and then can be used later, transferring pathogens to other surfaces. Ready-to-use wipes are kept in sealed containers until they are ready for use. When they are spent, they are discarded and a fresh wipe is dispensed, reducing the risk of cross-contamination.
Dwell time – This is the length of time that the surface must remain wet, with the disinfectant, in order to achieve the kill claims indicated on the label. Compliance can be a function of the disinfectant chemistry, the environmental component (i.e., heat or humidity) or the amount of disinfectant that is applied to the surface. Many dilutable disinfectants have unrealistic contact times, making it challenging for staff to achieve compliance with the label instructions. Ready-to-use disinfectant wipes often have shorter contact times, allowing for more frequent compliance with dwell time requirements.
Removal – Different cleaning tool substrates perform differently, and in many cases you can delineate this when measuring their ability to remove pathogens and soil. The effectiveness of the cloth is a function of the material, construction, and condition of the cloth. RTU disinfectant wipes provide you with a consistent cleaning substrate every time you dispense a new wipe.
Task Time – Since labor is the major component of any budget, it must always be taken into consideration when you are looking at total cost. Task time is defined as the time it takes to do a specific cleaning and disinfecting activity, and should encompass all components of the process. This includes dispensing or mixing of chemical, wetting the cloths for use, wringing, performing the task, changing out cloths, sorting cloths for laundering, and laundering time.
A recent study, published in Infection Control and Hospital Epidemiology (ICHE) by Dr. Timothy Wiemken and his colleagues from the University of Louisville, evaluated the impact of using ready-to-use (RTU) disinfectant wipes. When compared to the traditional towel and bucket method, RTU wipes significantly increased cleaning and disinfection compliance by 35%, decreased time to clean patient rooms by 23%, and reduced cost by $38.55 per employee per day. Click here for a link to his study.
Study Description: Researchers compared the use of the traditional towel and bucket method for cleaning and disinfection of hard surfaces in patient rooms to RTU disinfectant wipes. Nine employees participated in the study. Participants were randomly divided into two groups; 1) RTU wipes, and 2) towel and bucket. They were asked to clean six surfaces in each patient room. These surfaces were marked using a fluorescent marker, without the employee’s knowledge, prior to being cleaned. A scoring system was used to evaluate compliance (‘0’ was given if the marker was not removed, ‘1’ if the mark was partially removed, and ‘2’ if the mark was completely removed). The total cleaning time was measured using a stop watch. Cost savings were calculated based on the assumption that the employee wage was $10 per hour, 15 rooms were cleaned per day per employee, and that it took 20 minutes to clean each room.
Outcome: The average number of compliance points when using the RTU wipes was 10.6 as compared to 8.1 points for the cloth and bucket method (35% increase). The average time for completing the cleaning and disinfection of a room in the RTU group was 178.1 seconds vs. 230.9 seconds in the cloth and bucket group (23% decrease). The calculated cost savings per employee per day were $38.58.
Assuming that a hospital has 20 EVS employees who work 365 days a year, the total calculated savings would be: 20 X 365 X $38.58 = $281,634.
Editorial Conclusion: The authors concluded that the increased compliance with cleaning and disinfection practices, and the reduction in personnel time (labor costs) may be due to ease of use and the reduction in time required to obtain a new wipe vs. the time required to switch out towels when they become dry or contaminated. It is well known that compliance with cleaning and disinfection practice in acute care, operating rooms, and outpatient clinics is suboptimal which may contribute to an increase the risk of pathogen transmission. Based on this, the significant increase in compliance when using the RTU disinfectant wipes may contribute to a decrease in healthcare-associated infections, which may offset the increased cost of RTU wipes. Switching to RTU wipes may help healthcare facilities improve patient and employee satisfaction by eliminating the inefficiencies of the towel and bucket method.
The question remains… Are you ready to throw in the towel? If so, the era of the cloth towel may be gone, just like the handkerchief, replaced by an alternative that is more convenient, hygienic, and effective, that also eliminates the need for laundering. Throwing in the towel may be the best play you can make in your facility.

