General Information
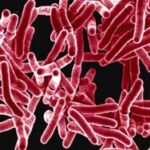
Mycobacterium tuberculosis is an infectious bacterium of concern that primarily affects the lungs. It causes what is known as Tuberculosis or TB. Spread between people is by person-to-person transmission through the air. Although the lungs are the primary site for infection, TB bacteria can attack other parts of the body such as the kidney, spine, and brain. People who have active TB will feel sick, have signs and symptoms, and may spread TB bacteria to others. If not treated properly, TB disease can be fatal.
Not everyone infected with TB bacteria becomes sick with TB disease. People who become infected but are not sick have what is called latent TB infection (LTBI). The bacteria are present in the person, but the immune system does not allow the TB bacteria to multiply. People who have LTBI generally do not display any of the signs or symptoms and cannot spread TB bacteria to others. But some people with LTBI go on to develop active TB, especially if their immune system becomes weakened due to age or immuno-suppression. It is important for persons diagnosed with LTBI to consult with healthcare providers and receive appropriate treatment to prevent future complications, including disease development and transmission to others.
How is TB transmitted?
Pulmonary tuberculosis is spread from one person to another through tiny, airborne particles released into the air when a person with an active case of TB coughs, sneezes, or when a person speaks or sings. People nearby may breathe in these bacteria. TB is NOT spread by direct human contact (shaking hands), sharing food or drink, or touching common surfaces.
Once a person inhales the TB bacteria it can enter the respiratory tract and make its way down into the lungs and can live there without causing active disease, sometimes for many years, without being able to transmit the bacteria to someone else. Notably, being exposed to a person with active pulmonary TB does not always result in subsequent infection.
When a person who has been exposed to the TB bacteria develops active infection, this is when they are able to transmit it to others. Active infection can develop when a person’s immune system becomes weakened because of other health issues as stated above.
Symptoms
The following signs and symptoms are associated with active infection:
- Coughing that has lasted for three weeks or greater
- Coughing up blood (also called hemoptysis) or sputum
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue or weakness
- Fever
- Night sweats
- Chills
- Loss of appetite
TB disease can also occur in other parts of your body. This is called extrapulmonary TB. Signs and symptoms vary according to the organs involved. For example, tuberculosis of the spine (in the spinal fluid) may give you back pain, and tuberculosis in your kidneys might cause blood in your urine. Per CDC, extrapulmonary TB is usually not infectious unless the following criteria are met:
- Pulmonary disease in addition to extrapulmonary disease;
- Extrapulmonary disease located in the oral cavity or the larynx; or
- Extrapulmonary disease includes an open abscess or lesion in which the concentration of organisms is high, especially if drainage from the abscess or lesion is extensive or drainage fluid is aerosolized.
Prevention in healthcare settings
Preventing the spread of pulmonary TB in healthcare settings is multifaceted and requires adherence to the facility-specific TB infection control program, policies and procedures. For guidance on facility-based TB risk assessments and infection control guidance, go to Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Settings, 2005.
Healthcare transmission-based precautions
In healthcare settings, airborne and standard precautions are required to prevent the spread of pulmonary TB, including a private airborne infection isolation room (AIIR) with proper air exchanges. Isolation placement is wholly dependent on healthcare providers’ astute and timely identification of TB signs and symptoms. Facility-approved respirators should be worn by healthcare professionals according to facility policy. If an AIIR is not available, patients/residents should be placed in a private room until proper accommodation can be made (e.g., transfer to a facility where AIIR is available, if indicated).
Are environmental surfaces a concern?
Pulmonary TB is spread via air currents, not environmental surfaces, but frequent cleaning and disinfection of environmental surfaces is an important aspect of all infection prevention and control.
Considerations for environmental cleaning and disinfection
Mycobactericidal pathogen kill claims on EPA-registered disinfectants are not required for the environmental cleaning and disinfection of surfaces where infected pulmonary TB persons receive care. In the 2005 TB prevention guidance references above, the CDC clarifies, “A common misconception in the use of surface disinfectants in health care relates to the underlying purpose of products labeled as tuberculocidal germicides. Such products will not interrupt and prevent transmission of M. tuberculosis in health-care settings, because TB is not acquired from environmental surfaces.”
When is using EPA-registered tuberculocidal disinfectants recommended in US healthcare settings?
In the early 1990s, the US Occupational Safety and Health Administration (OSHA) released guidance on dealing with the risk of occupational exposure to bloodborne pathogens. One of the requirements was that equipment and environmental surfaces be cleaned and decontaminated with an appropriate disinfectant after contact with blood or other potentially infectious materials. While the OSHA standard did not specify the type of disinfectant, it suggested that the disinfectant would be tuberculocidal to kill the hepatitis B virus (HBV). Thus, to be in regulatory compliance, a facility would have needed to use a tuberculocidal disinfectant to clean up a blood or other body fluid spill. In 1997, OSHA revised its policy and stated that any disinfectant effective against HIV and HBV or a disinfectant effective against TB would be effective for bloodborne pathogen cleanup.
A healthcare facility may prioritize using tuberculocidal disinfectants because the claim is used as a benchmark by which to measure overall germicidal potency. In other words, mycobacteria are the next most resistant microorganisms to kill after bacterial spores in the widely accepted hierarchy of disinfectants (McDonnell & Burke, 2011). However, tuberculocidal disinfectants are not a replacement for: EPA List K of sporicidal disinfectants, EPA List P for Candida auris, or EPA’s List Q for emerging viral pathogens. Just as sporicidal-level disinfection is not required in all healthcare spaces, nor is tuberculocidal-level disinfection, unless indicated by Spalding classification, the equipment manufacturer’s instructions for use, or the healthcare facility policies and procedures.
If EPA-registered disinfectants with tuberculocidal claims are requested, the following are available from Diversey:

References:
About Tuberculosis | Tuberculosis (TB) | CDC – www.cdc.gov/tb/about/
McDonnell G, Burke P. Disinfection: is it time to reconsider Spaulding? J Hosp Infect. 2011 Jul;78(3):163-70. doi: 10.1016/j.jhin.2011.05.002. PMID: 21664533.
Reviewed/Revised: August 2024

