Monkeypox
General Information
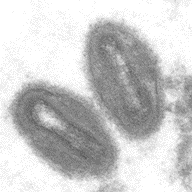
Mpox is a viral disease caused by the monkeypox virus (mpxv), which is part of the Orthopoxvirus genus of viruses, which also includes smallpox (variola virus). Mpox was first identified in 1958 in monkeys in Africa, and the first case human case was recorded in 1970 in the Democratic Republic of Congo (DRC). The virus is endemic (naturally found) in central and west Africa.
There are 2 types of mpxv- clade I and clade II. The first global outbreak, or public health emergency of international concern (PHEIC), was declared by the World Health Organization (WHO) from July 2022 to May 2023. This was caused by mpxv clade II which generally causes less severe infection and lower mortality than mpxv clade I. A second PHEIC was declared in August 2024. This global outbreak, caused by a new strain called mpxv clade 1b, is thought to be spread primarily by sexual contact and is associated with more severe illness and deaths. It has been detected in the DRC, in several neighboring countries, and now in countries outside of Africa.
Transmission:
Mpxv can spread through close contact (including intimate or sexual contact) with a person with mpox, through contact with contaminated materials and through contact with infected wild animals.
Person-to-person transmission of mpxv can occur through contact with infectious skin or lesions and includes:
- Direct skin to skin contact with mpox rash or scabs from a person with mpox
- Contact with saliva, upper respiratory secretions, and bodily fluids or lesions around the anus, rectum, or vagina from a person with mpox
- Intimate contact including
- Oral, anal, or vaginal sex, or touching the genitals (penis, testicles, labia, and vagina) or anus
- Hugging, massage, and kissing
- Prolonged face-to-face interactions (such as talking or breathing)
- Pregnant people with mpox can pass the virus to the fetus during pregnancy or to the newborn during and after birth.
Mpxv can be spread through contact with objects, fabrics and surfaces that have not been disinfected after use by someone with mpox. This includes items such as clothing and bedding.
Mpxv can spread from animals to people:
- Through small wild animals in West and Central Africa, where mpox is endemic
- Direct close contact with an infected animal, fluids or waste, or getting bitten or scratched.
- During activities like hunting, trapping, or processing infected wild animals in areas where mpox is endemic.
Symptoms:
Mpox can cause a painful rash on hands, feet, chest, face/mouth or near the genitals. Symptoms usually start within 3 weeks of exposure to the virus. The initial rash looks like pimples or blisters followed by scabs before healing. Other symptoms can include:
- Fever
- Chills
- Enlarged lymph nodes
- Exhaustion
- Muscles aches
- Headache
Symptoms typically last 2 to 4 weeks.
Diagnosis:
Specimens from skin lesion material (lesion surface, exudate or lesion crusts) should be collected for testing. Mpox is diagnosed using real time PCR tests which are available through local, state/provincial, territorial or tribal health departments and many large commercial laboratories. Only a trained physician should attempt to diagnose mpox as the presentation of signs and symptoms can be very similar to other infections. A physician can arrange for testing to conclusively diagnose mpox.
Infection Prevention in Healthcare Settings:
In addition to standard precautions, suspect or confirmed cases of mpox should be placed on contact precautions in a single room with the door closed and with a dedicated bathroom. Aerosol generating procedures, such as intubation and extubation, are likely to spread oral secretions and should be performed in an airborne infection isolation room.
Activities that could resuspend dried materials from lesions, such as use of portable fans and dry dusting, should be avoided. Care must be taken when handling soiled laundry (e.g., bedding, towels, personal clothing) to avoid contact with lesion material.
Healthcare workers should have access to personal protective equipment (PPE) including:
- Gown
- Gloves
- Eye protection (i.e., goggles or a face shield that covers the front and sides of the face)
- NIOSH-approved particulate respirator equipped with N95 filters or higher
Facilities should refer to their infection prevention and control policies for specific PPE requirements.
Waste management (i.e., handling, storage, treatment, and disposal of soiled PPE, patient dressings, etc.) should be performed in accordance with state/provincial and local regulations for handling, storage, treatment, and disposal of waste, including regulated medical waste.
Prevention:
Prevention measures include:
- Avoid skin to skin contact with people who have rashes that look like mpox and animals that carry mpox in endemic areas
- Isolation and appropriate medical care for those with suspected or confirmed mpox
- Avoid skin to skin contact with people who have been exposed to mpxv. Those exposed should seek medical care to determine the risk of infection and the need for potential interventions (such as quarantine, vaccination etc.)
- Avoid contact with objects and materials that a person with mpox has used
- Clean your hands often using soap and water or alcohol-based hand sanitizer
- Vaccination: People at risk of mpox should ideally be vaccinated prior to exposure. People may also be vaccinated after exposure to prevent developing mpox (i.e., post-exposure prophylaxis).
Environmental Cleaning and Disinfection:
Diligent environmental cleaning and disinfection and safe handling of potentially contaminated materials is important, especially if there are any body fluids. The CDC recommends that “activities such as dry dusting, sweeping, or vacuuming should be avoided. Wet cleaning methods are preferred.”
Soiled laundry (e.g., bedding, towels, personal clothing) should be handled in accordance with recommended standard practices, avoiding contact with lesion material that may be present on the laundry. Soiled laundry should be gently and promptly contained in an appropriate laundry bag and never be shaken or handled in manner that may disperse infectious material.
In the US, standard cleaning and disinfection procedures should be performed using an EPA-registered hospital-grade disinfectant with an emerging viral pathogen (EVP) claim. Products with EVP claims can be found on EPA’s List Q. According to the EPA, mpxv is a “tier 1 enveloped virus” which are the easiest to inactivate.
In Canada, use of a healthcare grade disinfectant with a Drug Identification Number (DIN) is required. Refer to Health Canada’s Surface Disinfectants for EVPs.
It is important to follow the manufacturer’s directions for concentration, contact time, and care and handling.
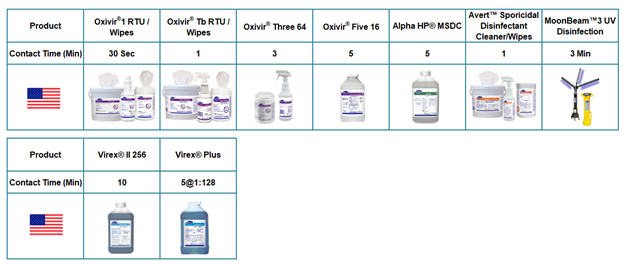
Below you will find products in the US with EVP Level 1 on List Q:
For Canada, there is a list for products with virucidal claims and the product would generally have a general (broad spectrum) virucidal claim. These are listed HERE by DIN (Drug Identification Number).
References:
- https://www.cdc.gov/poxvirus/mpox/about/index.html
- https://www.cdc.gov/poxvirus/mpox/clinicians/infection-control-healthcare.html#anchor_1653508869481
- https://www.cdc.gov/poxvirus/mpox/prevention/protect-yourself.html
- https://www.cdc.gov/poxvirus/mpox/symptoms/index.html
- https://www.canada.ca/en/health-canada/services/drugs-health-products/disinfectants/emerging-viral-pathogens.html#wb-auto-4
- https://www.epa.gov/pesticide-registration/disinfectants-emerging-viral-pathogens-evps-list-q
- Public Health Ontario Infection Prevention and Control (IPAC) Recommendations for Monkeypox in Health, Care Settings 2nd Revision: June 2022 https://www.publichealthontario.ca/-/media/Documents/M/2020/monkeypox-ipac-recommendations-healthcare-settings.pdf?rev=51039df4a87b4670948a681b1e0f2baf&sc_lang=en
- https://www.who.int/news/item/14-08-2024-who-director-general-declares-mpox-outbreak-a-public-health-emergency-of-international-concern#:~:text=The%20emergence%20last%20year%20and%20rapid%20spread%20of,main%20reasons%20for%20the%20declaration%20of%20the%20PHEIC.
- https://www.who.int/news-room/fact-sheets/detail/monkeypox#:~:text=The%20disease%20mpox%20%28formerly%20monkeypox%29%20is%20caused%20by,which%20includes%20variola%2C%20cowpox%2C%20vaccinia%20and%20other%20viruses.

